Clinical case scenario
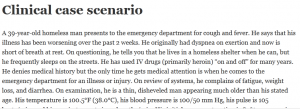
A 39-year-old homeless man presents to the emergency department for cough and fever. He says that his illness has been worsening over the past 2 weeks. He originally had dyspnea on exertion and now is short of breath at rest. On questioning, he tells you that he lives in a homeless shelter when he can, but he frequently sleeps on the streets. He has used IV drugs (primarily heroin) “on and off” for many years. He denies medical history but the only time he gets medical attention is when he comes to the emergency department for an illness or injury. On review of systems, he complains of fatigue, weight loss, and diarrhea. On examination, he is a thin, disheveled man appearing much older than his stated age. His temperature is 100.5°F (38.0°C), his blood pressure is 100/50 mm Hg, his pulse is 105 beats/min, and his respiratory rate is 24 breaths/min. His initial oxygen saturation is 89% on room air, which comes up to 94% on 4 L of oxygen by nasal cannula. Significant findings on examination include dry mucous membranes, a tachycardic but regular cardiac rhythm, a benign abdomen, and generally waste dappearing extremities. His pulmonary examination is significant for tachypnea and fine crackles bilaterally, but no visible signs of cyanosis. His chest x-ray is read by the radiologist as having diffuse, bilateral, interstitial infiltrates that look like “ground glass.”
Answer the following questions
What is the most likely cause of this patient’s current pulmonary
complaints?
➤ What underlying illness does this patient most likely have?
➤ What testing and treatment should be started now?